Your Lymphatic System: Important Facts:
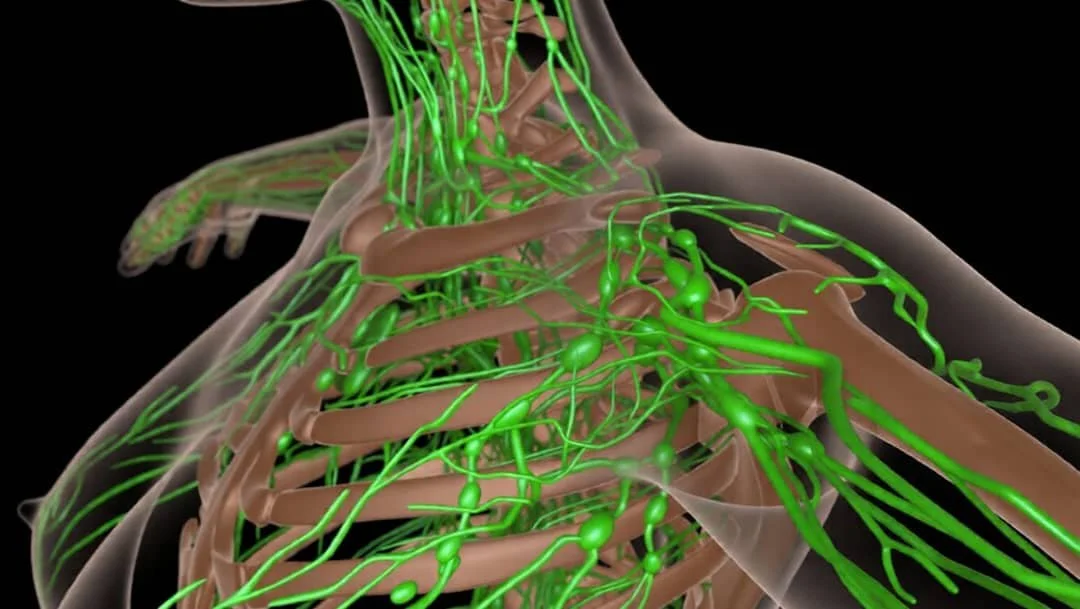
What does your lymphatic system do?
The lymphatic system is designed to:
Take away grime
Clear out toxins
Fight disease
Balance fluid levels (think puffy legs and face)
Transport nutrients and facilitate immunity In other words, it gets rid of the ugly things nobody wants to talk about.
The lymphatic system is also responsible for:
How quickly we can get in shape. Think metabolism, fat transportation, and the speed of hormonal responses.
How fast we recover from exercise. Removing lactic acid and cellular wastes.
How quickly we heal from sickness, surgery or injury, thanks to a quick-responding immune system
Summary:
When the lymphatic system is not working optimally swelling, fullness, puffiness, bloating, skin that feels tight and heavy and other such conditions manifest. This is called oedema or edema (US spelling). We call it lymphatic issues. From here, if left unattended lymphoedema and lipoedema can occur.
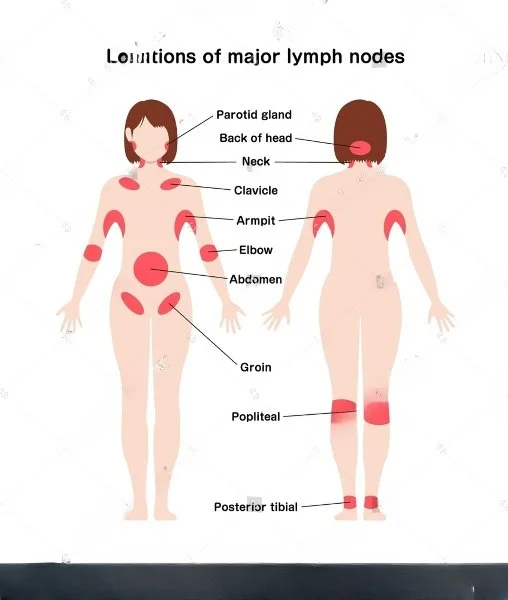
Where are the major lymph sites in the body:
Lymph nodes: Lymph nodes are bean-sized collections of lymphocytes and other immune system cells throughout the body. These nodes are located inside the chest, neck, abdomen, and pelvis. They are connected by a system of lymphatic vessels.
Spleen: The spleen is an organ under the lower ribs on the left side of the body. The spleen makes lymphocytes and other immune system cells. It also stores healthy blood cells and filters out damaged blood cells, bacteria, and cell waste.
Bone marrow: The bone marrow is the spongy tissue inside certain bones. This is where new blood cells (including some lymphocytes) are made.
Thymus: The thymus is a small organ behind the upper part of the breastbone and in front of the heart. It’s important in the development of immune cells, the T-lymphocytes
Adenoids and tonsils: These are collections of lymph tissue in the back of the throat. They help make antibodies against germs that are breathed in or swallowed.
Digestive tract: The stomach, intestines, and many other organs also have lymph tissue.
Appendix: The submucosa of the appendix contains many masses of lymphoid tissue, indicating a possible role in the lymphatic and immune systems.
Lymphatic issues cannot be cured. However the main symptoms including swelling and skin changes can be effectively managed.
The following questions have been answered using information produced and verified by accepted experts in their field and reflects current practice.
The information has been designed to assist you in managing your condition and is not intended to replace advice you may receive from your healthcare practitioner.
If you or your healthcare practitioner would like further information, to ask any questions about this information, to provide us with any feedback or to find out what research underpins it, please contact the Lymphatic Massage Academy on:
0410 63 7778.
Lymphoedema cannot be cured but the main symptoms including swelling and skin changes can be managed and effectively controlled. Most people who develop lymphoedema continue to lead very full and successful lives and learn how to successfully manage the long-term condition.
“Once it has developed can lymphoedema be cured?"
"Am I allowed to fly if I am at risk of developing lymphoedema?"
There is no evidence that flying either short haul or long haul will lead to lymphoedema developing. There is also no evidence to suggest that wearing any sort of preventative compression is needed or helps.
However, when flying, do take the following common sense precautions:
Do wear regular flight socks to prevent blood clots.
Keep moving your limbs as much as you are able during the flight – particularly the ‘at risk’ limb.
Wear loose fitting clothes, shoes and jewellery to travel in.
Keep well hydrated during and after the flight (water, not alcohol!).
“What can I do to reduce the risk of developing lymphoedema?”
As we do not know why some people go on to develop lymphoedema and others do not, please remember that while it is sensible to do all you can to try and reduce the risk, it is equally important to live your life in the fullest way possible and not to feel guilty that you have caused the swelling if it should develop.
Weight management:
Gaining weight and being overweight is one of the biggest risk factors in developing lymphoedema. In order to reduce that risk, it is important to maintain a good healthy diet, exercise regularly and do all you can to keep your weight within normal limits. The LSN has a leaflet with further information on healthy eating. The following may also be useful to you.
Movement and exercise:
Gentle movement, exercise and activities will help the muscles pump lymph fluid through your body.
Movement helps to improve and maintain flexibility and keeps your bones strong.
Being active helps you achieve and maintain a healthy weight and may well improve your emotional wellbeing.
Some studies suggest that doing exercise may help prevent your cancer returning.
Any movement that stimulates the muscles is beneficial. Try to do a little every day and build up gradually. Remember to pace yourself and listen to your body.
Activities such as walking, swimming, cycling, gardening, yoga and Pilates can all be helpful.
If you notice an activity causes increased aching, swelling or feelings of heaviness in your limb either immediately after or in the days following the activity, reduce the intensity or try some other form of movement.
Did you know that your lymphatic vessels need to inflame by more than 100 per cent before being noticed!
This is how this inflammation can show up:
Joint pain
Hands and feet pain
Itchiness
Breast swelling
Cellulite
Chronic fatigue
Swelling of lymph nodes in the throat, armpits or groin
Muscle aches and pains
Sore throats
Hormonal problems
Haemorrhoids
Weight gain
Sickness and disease
Stress.
“How does lymphatic imbalance show in your body?”
The following has been known to slow down and block-up this major lymphatic and glymphatic transport system..(Its a long list )…
Coffee
Sugar
Dairy
Processed foods
Cleaning products
Prescription drugs
Alcohol
Surgery
Acidic foods
Pesticides
Stress
Beauty products
Tattoo ink
Making the connection between what your body consumes to how you feel every day, as well as lifestyle factors, is the key to your wellness. If you aren’t feeling so great (fatigue, bloating, excess weight, brain fog, acid reflux, constipation, skin issues, allergies, pain, and inflammation) ask yourself why. Consider what you can do to reduce or remove it from your lifestyle?
Picture all of your cells living in this 15L of lymphatic fluid. This is where they receive their nutrition, energy and support. How well do you look after your cells?
Do you:
Drink at least two litres of water a day?
Move your body?
Breathe deeply?
Or do you:
Wear restrictive clothes
Have broken sleep
Consume/use some of the damaging products above
Feel toxic
Are you just hanging in there … surviving and not thriving?
By targeting your lymphatic health, you will be better supporting every system in your body.
By looking at the lymphatic system, rather than getting caught up in the individual disease or diagnosed symptom, you can make big changes in your life. Best of all, you can do it yourself at home. All you have to do is follow some very simple (and fun) steps.
How?
Our signature three day Lymphatic Massage intensive is easy enough to learn. You will also have access to the ongoing support of our team.
Our approach includes many traditional therapies that I have used for nearly 30 years in clinical application.
“What are the main things that badly affect lymphatic health? "
Information for Health Practitioners:
Once an assessment has been carried out and a diagnosis of chronic oedema or lymphoedema or a lymphatic issue has been made, the patient should be referred for specialist treatment as soon as possible to prevent further complications such as skin damage, leakage and infection. Whilst lymphatic issues are not a medical emergency, the earlier treatment is commenced the easier it is to minimise its severity and associated complications.
Lymphatic issues, Lymphoedema and Chronic Oedema are long-term conditions and those living with it will need ongoing, holistic management and support. Professor Peter Mortimer, a leading lymphoedema specialist in the UK, states that all patients with chronic swelling should expect:
An explanation about the most likely cause of their chronic swelling
Prompt referral to a lymphatic practitioner
A treatment programme incorporating the four cornerstones of lymphatic treatment as appropriate
Ongoing care according to accepted standards
The option of additional treatment at intervals as needed
Whilst ultimately you may not be the health care professional providing ongoing care for those with lymphatic issues in your practice, there is some helpful general advice which you can offer your patients once an assessment and diagnosis of a lymphatic issue, lymphoedema/chronic oedema has been made.
Patients should:
Try to use the affected limb as normally as possible as muscle activity will encourage lymph drainage
Try to keep their weight within normal limits
Drink plenty of fluids and avoid taking diuretics unless they have another medical condition that requires them to do so. Diuretics are not recommended for routine use in simple lymphoedema. Occasionally they are of benefit where there may be more than one cause of swelling, but when diuretics are prescribed their efficacy should be monitored and if there is no resolution of the swelling then the diuretic should be stopped and specialist advice sought
Keep their skin clean, moisturised and in the best possible condition, avoiding injections/needles, blood tests and blood pressure readings on the affected limb, whenever possible
Everyone who lives with lymphatic issues are different and their experience of the condition is unique but there are four specific areas of treatment that may be used to create an individual plan for your patients.
i) Lymphatic drainage massage/ Manual Lymphatic Drainage (MLD) – this is a special massage technique aimed at moving fluid out of the affected area.
This massage should only be carried out by specially trained practitioners, but a simplified form (SLD) can be taught to patients and/or their partners/carers.
ii) Skin Care – to keep the skin in good condition and reduce the risk of infection (cellulitis).
iii) Exercise – is essential to maximise lymph drainage, keep the body supple and weight within normal limits.
iv) External compression – this supports the area, assists in reducing the overall swelling, improves shape and helps prevent further build-up of fluid. Initially, this may be done by applying a specialised form of bandaging, but more often will mean wearing prescribed elastic graduated compression garments. It is important that these garments are the correct compression and size.